Understanding the Endotracheal Tube and Its Clinical Use
Published on: August 16, 2024
Introduction
In medical emergencies, particularly those involving respiratory distress or compromised airways, the endotracheal tube (ET tube) plays a pivotal role in patient care. It is a lifesaving device that allows clinicians to maintain an open airway, deliver oxygen, and perform ventilation effectively. Understanding the ET tube’s structure, functions, and the correct methods of use is fundamental for any healthcare professional involved in critical care, anesthesia, or emergency medicine.
Endotracheal intubation is not only about placing a tube in the trachea; it involves a series of steps that require precision, knowledge of anatomy, and familiarity with the equipment. This guide will walk you through the essentials of endotracheal tubes, their clinical applications, and the techniques for successful intubation.
Table of Contents
- What is an Endotracheal Tube?
- Types of Endotracheal Tubes
- Indications for Endotracheal Intubation
- How to Use an Endotracheal Tube: The Intubation Process
- Common Complications Associated with ET Tubes
- Frequently Asked Questions (FAQ)
- Conclusion
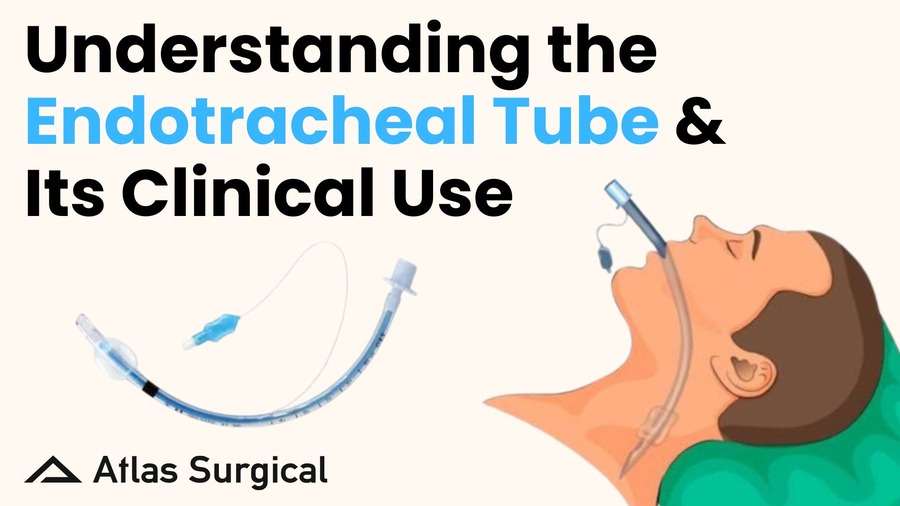
What is an Endotracheal Tube?
An endotracheal tube (ET tube) is a flexible plastic tube inserted through the mouth (orotracheal) or nose (nasotracheal) into the trachea to maintain an open airway. This tube serves as a conduit for oxygen, anesthetic gases, or medications to reach the lungs directly, bypassing any obstructions in the upper airway.
- Structure of an ET Tube: The ET tube is typically made from polyvinyl chloride (PVC) and comes in various sizes, from 2.0 mm to 10 mm in internal diameter...
- Cuff and Pilot Balloon: One of the most critical components of an ET tube is the cuff...
- Markings and Depth Indicators: ET tubes are marked with depth indicators...
Types of Endotracheal Tubes
There are several types of endotracheal tubes, each designed for specific clinical scenarios...
- Cuffed vs. Uncuffed ET Tubes: Cuffed ET Tubes are most commonly used in adults...
- Orotracheal vs. Nasotracheal Tubes: Orotracheal tubes are inserted through the mouth...
- Reinforced (Armored) ET Tubes: These tubes have a wire-reinforced wall...
- Endobronchial (Double-Lumen) Tubes: Used in thoracic surgery, these tubes allow ventilation of one lung...
Indications for Endotracheal Intubation
Endotracheal intubation is indicated in various clinical scenarios...
- Airway Protection: Patients who are unable to protect their airway due to altered mental status...
- Respiratory Failure: Patients with respiratory failure may require intubation...
- General Anesthesia: Intubation is performed to maintain airway patency during surgeries...
- Trauma and Emergency Situations: In trauma settings, patients may require intubation to secure the airway...
- Prevention of Hypoxemia: In patients with conditions that might lead to sudden hypoxemia...
How to Use an Endotracheal Tube: The Intubation Process
Endotracheal intubation is a step-by-step process that requires skill and precision...
1. Preparation: Assemble all necessary equipment, including the laryngoscope, ET tube...
2. Patient Positioning: Position the patient in the “sniffing” position...
3. Performing Laryngoscopy: Insert the laryngoscope in your left hand and advance the blade...
4. Inserting the ET Tube: Once the vocal cords are visualized, pass the ET tube...
5. Securing the Tube: Once placement is confirmed, secure the tube with tape or a tube holder...
Common Complications Associated with ET Tubes
Despite its life-saving benefits, endotracheal intubation carries potential risks...
- Tube Misplacement: Misplacement of the ET tube, either in the esophagus or a mainstem bronchus, is a common complication...
- Trauma to the Airway: Insertion of the ET tube can cause trauma to the airway...
- Aspiration: If the tube is not correctly positioned, the patient is at risk of aspiration...
- Ventilator-Associated Pneumonia (VAP): Prolonged intubation increases the risk of developing VAP...
Frequently Asked Questions (FAQ)
1. What size endotracheal tube should be used for adults?
The appropriate ET tube size for adults generally ranges between 7.0 mm and 8.0 mm for females, and 8.0 mm to 9.0 mm for males. The exact size depends on the patient's airway anatomy and clinical condition.
2. How is the correct placement of an endotracheal tube confirmed?
Correct placement is confirmed by auscultating bilateral breath sounds, observing chest rise, and using a CO2 detector to verify end-tidal CO2.
3. What are the risks of prolonged intubation?
Prolonged intubation can lead to complications such as ventilator-associated pneumonia (VAP), tracheal stenosis, and injury to the vocal cords or tracheal mucosa.
4. Can children be intubated with cuffed endotracheal tubes?
Yes, cuffed endotracheal tubes are increasingly being used in pediatric patients to ensure effective ventilation, but care must be taken to avoid excessive cuff pressure, which can damage the trachea.
5. What is the difference between orotracheal and nasotracheal intubation?
Orotracheal intubation is performed through the mouth and is commonly used in emergencies, while nasotracheal intubation is performed through the nose and is used when oral access is restricted, such as in maxillofacial surgery.
Conclusion
The endotracheal tube is an essential tool in critical care, anesthesia, and emergency medicine. Its role in maintaining an open airway, delivering oxygen, and providing ventilation cannot be understated. However, it requires proper knowledge and skill to use effectively and safely. Understanding the types of ET tubes, indications for use, and correct intubation techniques is vital for all healthcare professionals working in acute care settings.
For more information on airway management and related products, visit the Endotracheal Tube section on our website.